Pelvic Organ Prolapse
Jun 21, 2023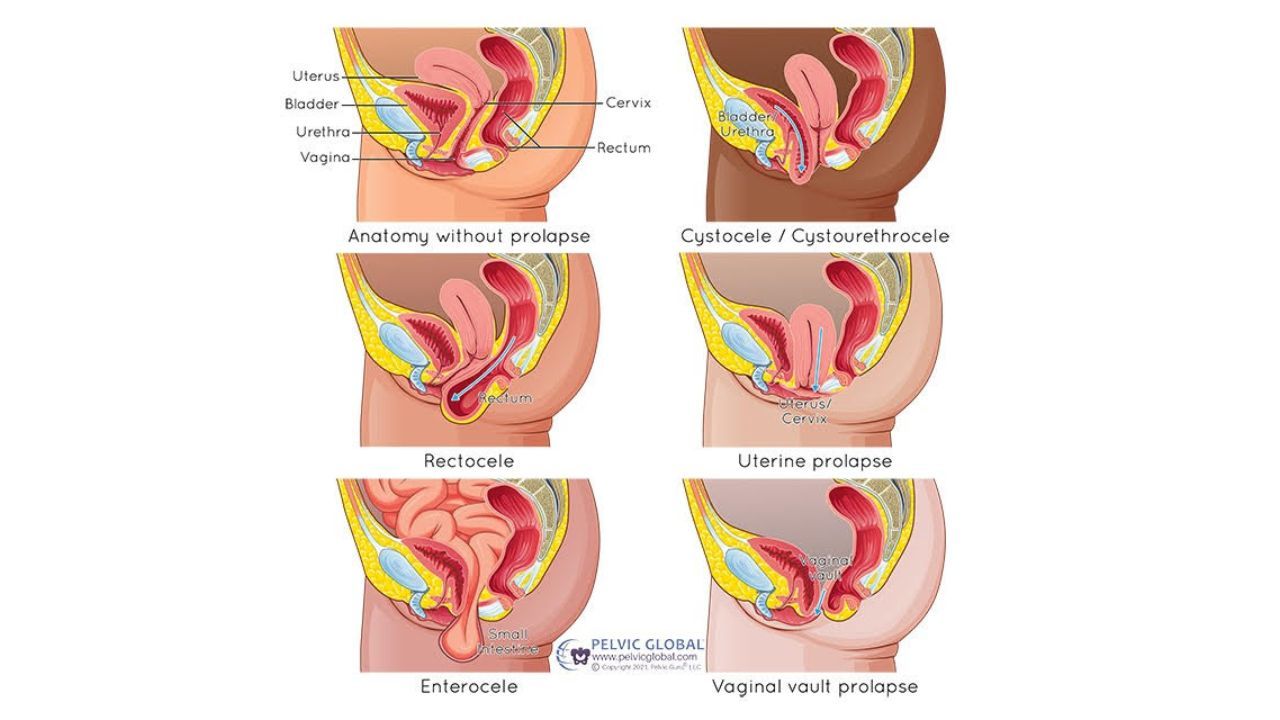
This information is about pelvic organ prolapse: different types, symptoms and management options
Usually the first sign someone gets regarding pelvic organ prolapse is being able to see or feel tissue in the vaginal canal. Without background knowledge of what this is or what it means, it can be very upsetting and isolating.
I'm here to tell you that a pelvic organ prolapse diagnosis does not automatically mean you do nothing, wait, and then have surgery. Far from it.
Pelvic Floor Physical Therapy can help improve prolapse and teach you how to manage prolapse moving forward so that it's not even a thought, let alone a worry in your brain.
Also, if you are at the point where your prolapse does require surgical intervention, having an appointment with pelvic floor physical therapy prior to surgery can help teach you how to use your muscles effectively and manage pressure through your body to prevent a reoccurrence of pelvic organ prolapse!
WHAT IS PELVIC ORGAN PROLAPSE
This is when the pelvic organs start to descend down into the vaginal canal or rectum.
DIFFERENT TYPES
Bladder (Cystocele) - bladder tissue presses on the front of the vaginal wall
Rectum (Rectocele) - the rectum presses into the back of the vaginal wall
Uterus (Uterine prolapse) - uterus lowers down the vaginal canal
Small Intestines (Enterocele) - possible after hysterectomy (removal of the uterus), small intestine tissue presses into the vaginal vault
Urethra (Urethrocele) - urethra presses down on the front of the vaginal wall and usually happens with a cystocele
POSSIBLE SYMPTOMS:
Low back pain
Heaviness or pressure in the pelvis
Sensation of something in the vaginal canal
Difficulty emptying bladder or urinary leakage
Bulge of tissue at the vaginal opening
Feeling of needing to press up on perineum (area between vaginal and rectal openings) to have or assist a bowel movement
INTERESTING FACTS:
Up to 50% of women have some degree of pelvic organ prolapse upon exam, with or without symptoms.
Pelvic floor muscle tightness can create the appearance and sensation of pelvic organ prolapse.
Ligament laxity and fascial stretching in the vaginal canal can contribute to pelvic organ prolapse.
Release work can greatly and positively impact pelvic organ prolapse.
PROLAPSE MANAGEMENT OPTIONS:
If constipated, work on bowel regularity without the need to strain.
Pelvic floor muscle awareness.
Decrease pelvic floor muscle tightness and increase pelvic floor strength through it's full range of motion.
Improve strength and function in the entire body to support a healthy pelvic floor.
Training including using your pelvic floor muscles properly for activities that increase pressure downward such as coughing, sneezing, laughing, lifting and more.
Stand and sit tall to avoid pressure. Slouching and slumping over time leads to more downward pressure on the pelvic organs.
Pessaries help to provide support to the vaginal walls. There are many different sizes, types, and ways to use them.
Surgical repair.
If you think you may have pelvic organ prolapse, know you have pelvic organ prolapse, or would like to learn how to prevent having pelvic organ prolapse in the future, click below to schedule a visit. A referral is not required unless you need or want physical therapy longer than 30 days.
Ready to schedule an appointment? Click below to get started today.
Get my Guide to Better Bladder and Bowel Health plus information about peri and postmenopause by signing up below!
Don't worry, your information will not be shared and you can unsubscribe at any time! (But why would you want to? :)


